Advocating for Yourself: L. Marie’s Experience with PBC

L. Marie started her career more than 20 years ago helping others access community health programs and healthcare—a skillset she never imagined would eventually be put to use advocating for her own health after being dismissed by her doctors.
It was January 2019 when L. Marie first sensed that something was wrong. She felt much more tired than normal, but chalked it up to the weather—thinking that the cold, dark winter days in Chicago were responsible for her feeling of being rundown.
“As women, we can explain away anything,” says L. Marie. “It took me a while to come to terms that there was something going on and that I needed to start looking for answers.”
When she visited her doctor, she was frustrated that her symptoms were discounted, even after her blood work came back irregular.
“How active are you?” “What’s your diet like?” were the questions her primary care physician asked, dismissing the serious fatigue L. Marie had been experiencing for weeks.
“As givers and caretakers—at home and at work—women give so much, but this was a moment in my life when I finally said, ‘wait a minute, I need to focus on me right now.’”
The fatigue persisted, but so did L. Marie. After pressing her doctor to run more tests, they noticed that she had elevated alkaline phosphatase (ALP) levels which can indicate liver disease or certain bone disorders.1 But an MRI and bone scan confirmed that her bones were strong, and she knew she needed to find out more about liver diseases.
Luckily, L. Marie’s health insurance didn’t require a referral to see a specialist and after doing some research on her own, she made an appointment with a hepatologist. Given her career, she knew how to navigate the healthcare system and within a week, L. Marie was finally in front of a specialist who would be able to give her answers. The diagnosis was primary biliary cholangitis (PBC), which was later confirmed with a liver biopsy, and validated what she had known from the beginning: something was not right.
PBC is a rare, progressive autoimmune cholestatic liver disease in which bile ducts in the liver are gradually destroyed and can inhibit the liver’s ability to rid the body of toxins.2 It is also a disease that predominantly affects women.3
Accepting and Giving Support
“When you’re first diagnosed, you’re thirsty for knowledge,” recalls L. Marie. Unfortunately, she didn’t get support resources from the doctor who diagnosed her – she was instead told to do her own research. She took a proactive approach and reached out to the American Liver Foundation who connected her with a local PBC group.
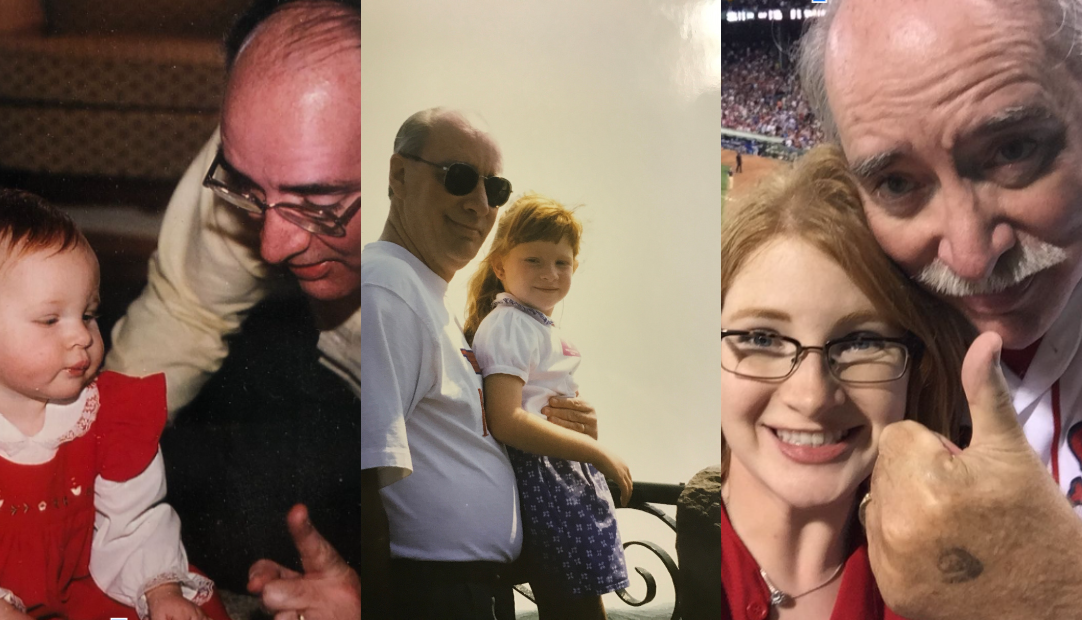
“There are two dates you remember,” L. Marie reflects on her experience. “The day you were diagnosed and the day you met another person living with PBC. The better day is meeting someone else with PBC because you realize you’re not alone. People living with PBC are all different, and come from different walks of life, different generations, but there is something underneath that links us together—it’s like a sisterhood.”
While L. Marie still finds support among her close friends and family, she takes comfort in knowing she’s not alone. That there are others who are living with PBC and who understand what it’s like to navigate an “invisible” disease and the challenges that come with it.
The Credibility Gap
L. Marie’s story, like so many others, reflects the inherent bias in our healthcare system, especially the inequity that exists for women’s health.
Research shows that women and racial and ethnic minorities are up to 30 percent more likely to be misdiagnosed than white men.4 Women’s health concerns are often chalked up to “daily life” as a caretaker for their family or can be blamed on mental health, weight or lack of diet and exercise. These generalizations not only are dismissive to potential underlying conditions, which can lead to delays in diagnosis and effective treatment, but create a dynamic where someone may not bring up the realities of how they are feeling or even fuel stigmas that exist.
For people with PBC, studies have indicated that because some of the symptoms—like itching and fatigue—are “invisible” there is a fear of being viewed as complaining about the burden or impact of disease on daily life.5
Moving Forward
For L. Marie, she has become the CEO of her own health. She speaks about her experience in hopes of empowering others to do the same. In many ways, she approaches this facet of her life like she does her career.
“This condition isn’t going away,” says L. Marie. “I need to know how I can educate myself and plan for the future while helping others do the same.”
Thankfully, L. Marie was diagnosed with PBC early with her self-advocacy, but there are many others who are not. She hopes that others will have the courage and feel empowered to not give up when advocating for themselves with their healthcare provider and when necessary, to break down the barriers that exist within our healthcare system.
For women who may feel overlooked or ignored by the health system, L. Marie encourages you to “be unwavering in your commitment to advocate for yourself. You know your body best and you deserve answers.”
1https://my.clevelandclinic.org/health/diagnostics/22029-alkaline-phosphatase-alp
2Kimagi T, et al.. Orphanet J Rare Dis. 2008; 3:1
3Galoosian A, et al. 2020. Clinical updates in primary biliary cholangitis: trends, epidemiology, diagnostics, and new therapeutic approaches. J Clin Transl Hepatol. 8(1), pp. 49-60.
4https://qualitysafety.bmj.com/content/33/2/109