How physicians can help empower people living with Primary Biliary Cholangitis
During the European Association for the Study of the Liver (EASL) congress, leading liver experts, Dr Mark Swain, Dr Emma Culver, and Dr Marco Carbone, sat down to discuss the effective management of primary biliary cholangitis (PBC). The conversation covered topics including the importance of regular medical check-ups, a personalized care approach, and a shared responsibility for disease management between doctors and patients who are living with PBC.
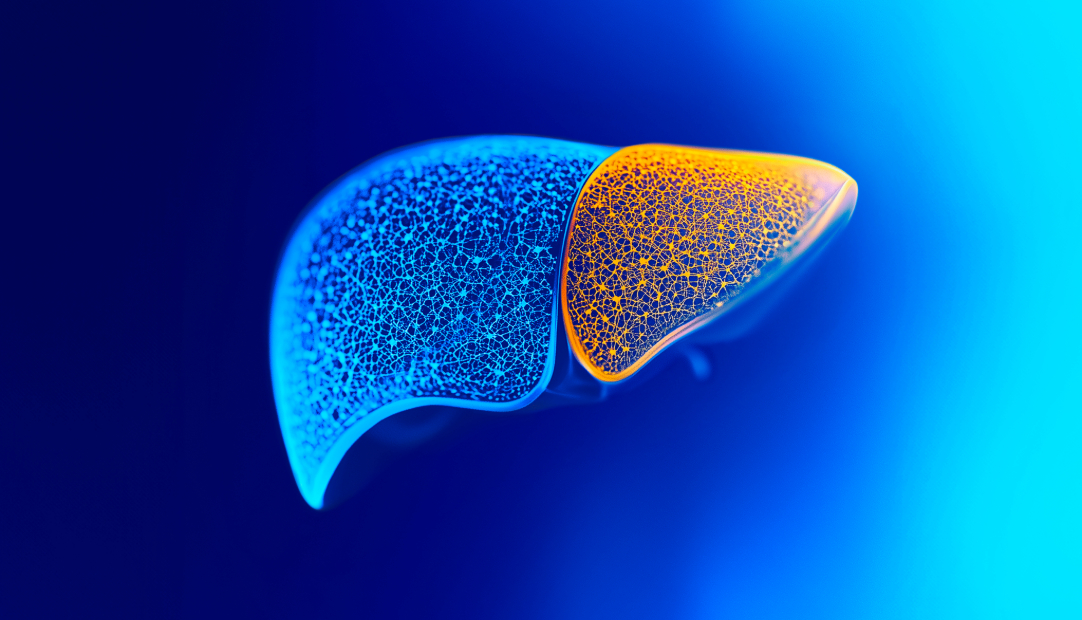
PBC is a rare and progressive autoimmune cholestatic liver disease, with an increasing worldwide prevalence.1-4 PBC can cause chronic inflammation of the bile ducts, leading to a build-up of bile and toxins in the liver (cholestasis), which results in scarring of the liver tissue (fibrosis) which can lead to cirrhosis. If left untreated or under-managed, PBC can eventually lead to liver failure.5,6
The importance of considering a holistic approach to patient care, to manage both symptoms and disease progression, was discussed. With agreement that educating patients about the relevance of liver blood tests and helping patients to understand the importance of managing biomarkers of PBC progression, such as alkaline phosphatase (ALP) and bilirubin, can help patients be in charge of the condition they live with.
The experts considered how the overall goal of a consultation is to ensure that patients’ concerns are fully addressed. Symptoms such as fatigue, itching, and dry eyes/mouth, are often under-recognized and under-treated, despite having a significant impact on the daily lives of people living with PBC. Ensuring that doctors listen to the symptom impact on quality of life and respond with appropriate advice, was emphasised in the discussion.
It was agreed that patients and their doctors need to meet for regular consultations at least every six to twelve months. During these consultations, patients should be given the opportunity to discuss the status of their disease in terms of ALP and bilirubin levels, and the impact of their symptoms on their quality of life.
It was concluded that doctors that support a shared management approach, who listen to patients’ needs and involve them in decision-making, contributes to the empowerment of patients to manage their disease.
References
- Lv T, et al. J Gastroenterol Hepatol. 2021;36(6):1423–1434.
- Galoosian A, et al. J Clin Transl Hepatol. 2020;8(1):49-60.
- Lindor KD, et al. Hepatology. 2019;69(1):394-419.
- Kumagi T & Heathcote EJ. Orphanet J Rare Di. 2008;3:1.
- Younossi ZM, et al. Am J Gastroenterol. 2019;114(1):48–63.
- Hirschfield GM, et al. Expert Rev Gastroenterol Hepatol. 2021;15(8):929-939